Less is more for health and happiness
- …


Less is more for health and happiness
- …


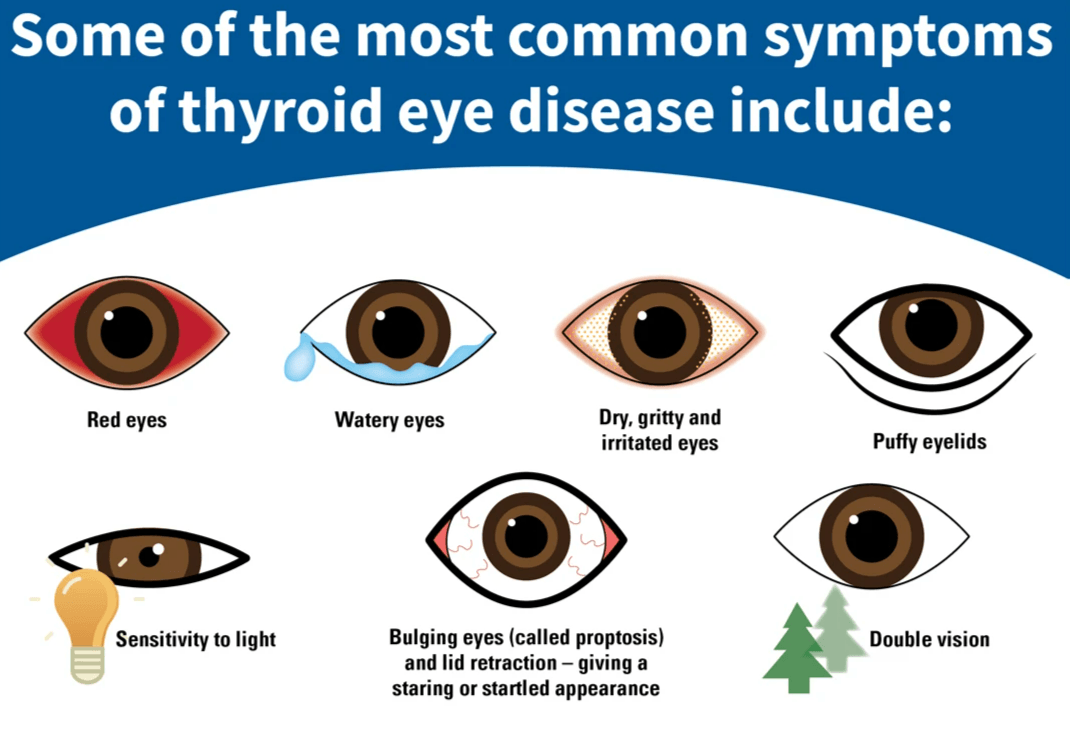
Diagnosing TED involves a careful clinical assessment that looks at both the signs and symptoms patients present with. Common symptoms include grittiness, eye watering, aching, and double vision (diplopia). On examination, doctors may observe ocular injection (redness), periocular swelling, proptosis (bulging eyes), lid retraction, and sometimes strabismus (misalignment of the eyes).
A key tool used in diagnosis is the Clinical Activity Score (CAS), which helps clinicians assess the level of inflammation and activity of the disease. This scoring system is widely used in Europe and recommended in consensus guidelines for monitoring TED.
Additionally, ensuring the patient’s thyroid function is well controlled (achieving euthyroidism) is an important part of the diagnostic process, as TED is closely related to thyroid abnormalities.
Since TED can vary in severity—from mild symptoms that still impact quality of life to sight-threatening complications—early recognition and a multidisciplinary approach involving endocrinologists and eye specialists are essential for optimal care.
Activity and severity definitions for patients with thyroid eye disease
A. Activity
1. Clinical activity score
The 7-item clinical activity score (CAS) is shown hereunder. Each item scores 1 point if presenta
- Spontaneous retrobulbar pain
- Pain on attempted up or lateral gaze
- Redness of the eyelids
- Redness of the conjunctiva
- Swelling of the eyelids
- Inflammation of the caruncle and/or plica
- Conjunctival edema, also known as chemosis
2. Active TED
A CAS ≥ 3/7 usually implies active TED. A history or documentation of progression of TED based on subjective or objective worsening of vision, soft tissue inflammation, motility, or proptosis is suggestive of active TED independently of the CAS.
3. Inactive TED
Patients usually enter the inactive phase 12–18 months after disease onset. Although improvement in signs and symptoms occurs during this period, proptosis and extraocular muscle dysfunction frequently do not normalize without intervention and may persist in up to 50% of patients.
B. Severity
1. Sight-threatening TED
Patients with dysthyroid optic neuropathy (DON) and/or corneal breakdown and/or globe subluxation.
2. Moderate-to-severe TED
Patients without sight-threatening disease whose eye disease has sufficient impact on daily life to justify the risks of medical or surgical intervention. Patients with moderate-to-severe TED usually have any one or more of the following: lid retraction ≥2 mm, moderate or severe soft tissue involvement, proptosis ≥3 mm above normal for race and sex, or diplopia (Gorman score 2–3).
3. Mild TED
Patients whose features of TED have only a minor impact on daily life insufficient to justify immunosuppressive or surgical treatment. They usually have only one or more of the following: minor lid retraction (<2 mm), mild soft tissue involvement, proptosis <3 mm above normal for race and sex, transient or no diplopia, and corneal exposure responsive to lubricants.
Reference: Burch, H. B., Perros, P., Bednarczuk, T., Cooper, D. S., Dolman, P. J., Leung, A. M., Mombaerts, I., Salvi, M., & Stan, M. N. (2022). Management of thyroid eye disease: a Consensus Statement by the American Thyroid Association and the European Thyroid Association. European Thyroid Journal, 11(6), e220189. Retrieved Jul 5, 2025, from https://doi.org/10.1530/ETJ-22-0189
Add paragraph text here.
Routine Eye Exams
Some people already know they have the related thyroid condition, Graves' disease. They aren't surprised when they get their first eye symptoms. Eye problems often appear within 6 months of a Graves' disease diagnosis. Once you know you have Graves’ disease, it's important to keep up with your eye doctor visits. It might be in a routine visit with your eye doctor that the path towards a diagnosis of thyroid eye disease begins.
Your eye doctor will do regular exams. During these checkups, they will ask whether you've had any vision problems and will look for symptoms such as:
- Swelling in and around your eyes
- Eyelid openings that are wider than normal
- Bulging eyes
- Misaligned eyes that don’t seem to focus on the same object at once
Your eye doctor will also check your vision. This may include tests of your color vision, as well as your central and side (peripheral) vision. The doctor will also measure your eyelids. Thyroid eye disease can make them swell or pull back.
In some cases, eye symptoms show up a few months before Graves' disease symptoms. If you didn't know you had a thyroid disorder, the sudden appearance of puffy eyelids, double vision, a gritty feeling in your eyes, or light sensitivity might send you to your eye doctor in search of answers.
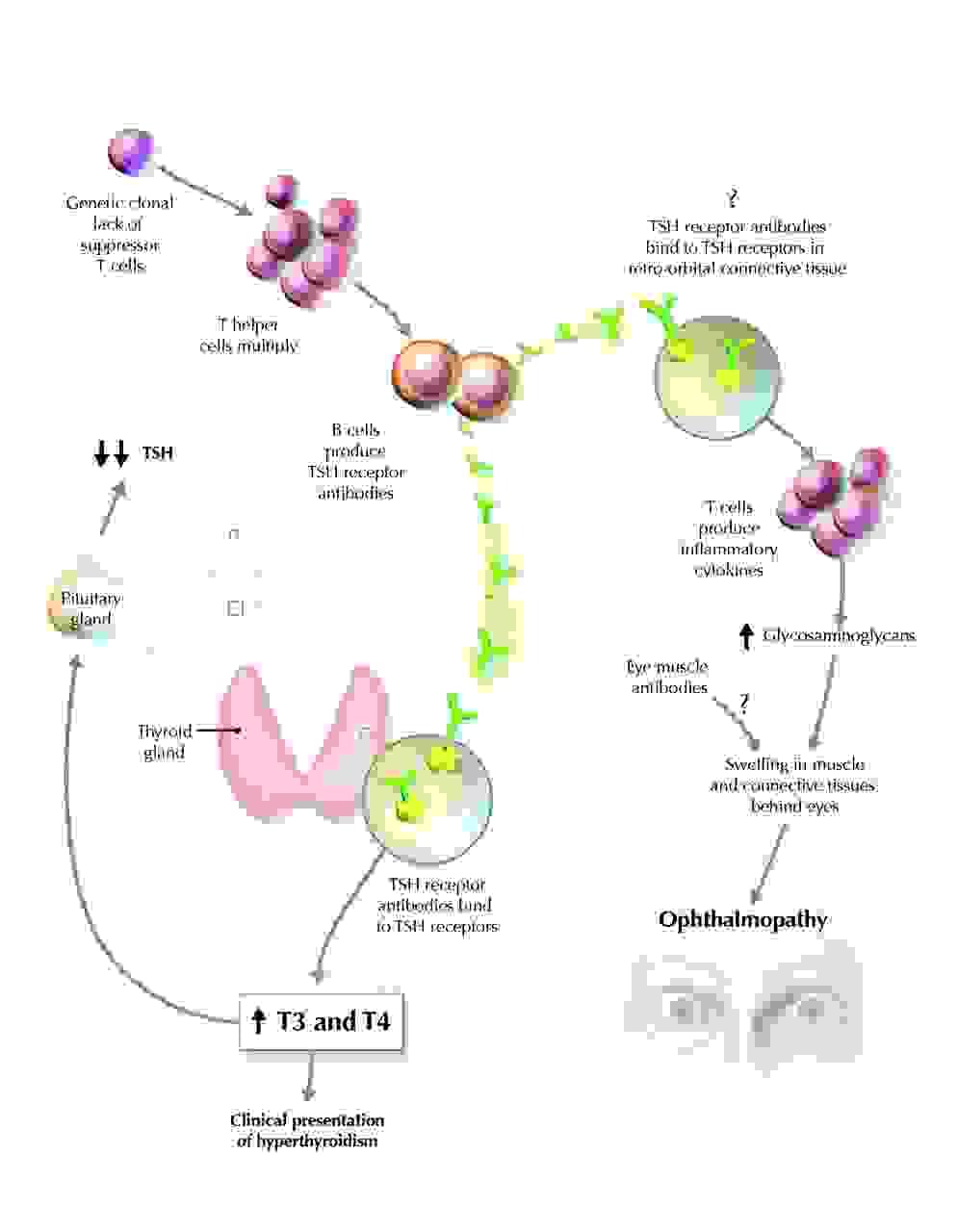
Pathogenesis of Graves' ophthalmopathy
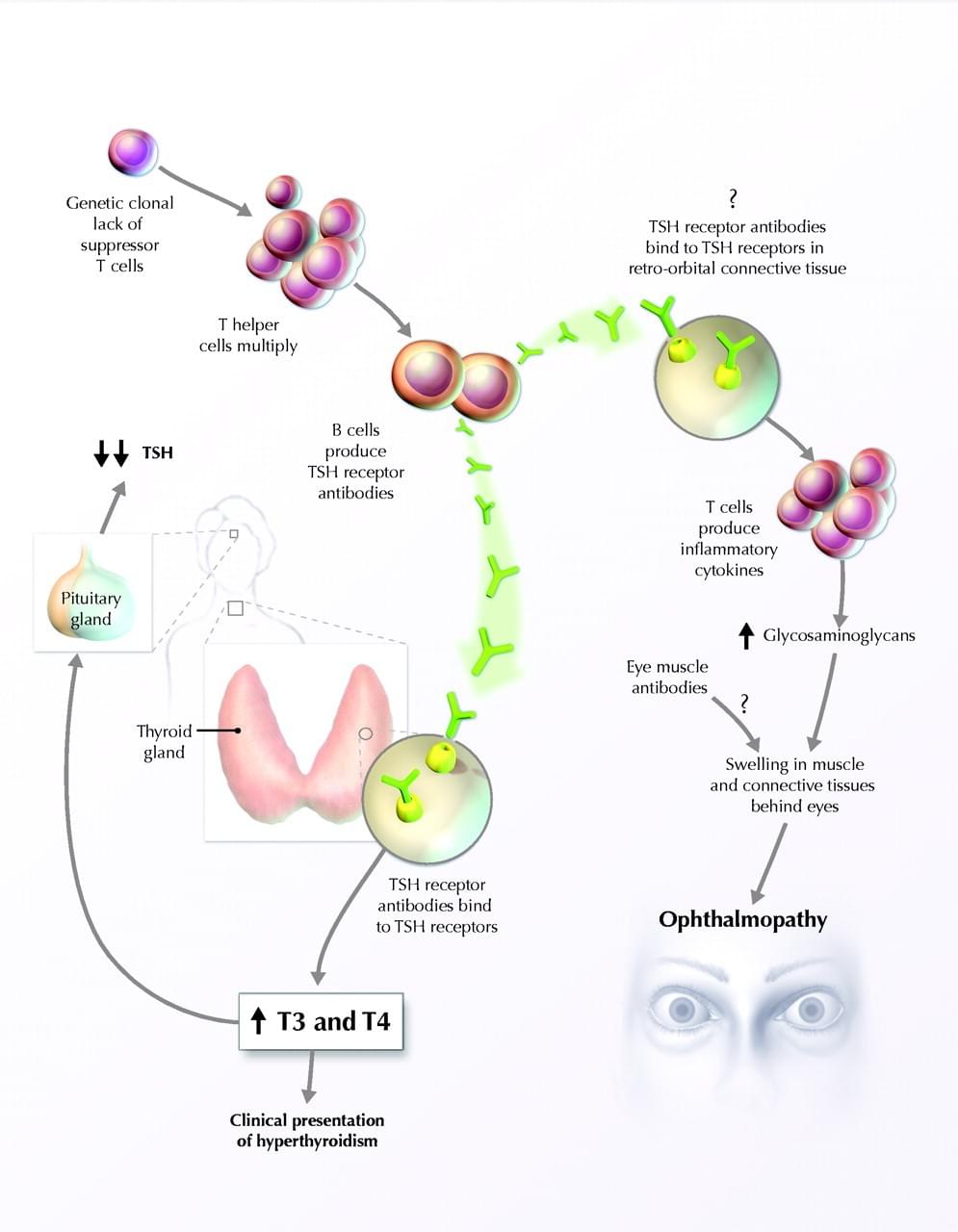
TED – also known as Graves’ Orbitopathy or Ophthalmopathy – is an autoimmune condition. It occurs when the body’s immune system attacks the tissue around and behind the eye, causing inflammation in the tissues. In most patients, the same autoimmune condition that causes TED also affects the thyroid gland, resulting in Graves’ disease. Usually this can be confirmed with a blood test to measure TSH Receptor Antibodies (TRAbs.) Graves’ disease most commonly causes thyroid overactivity (hyperthyroidism) but can also rarely cause thyroid underactivity (hypothyroidism).
TED can occur in people when their thyroid is overactive, underactive or functioning normally. It can also occur after treatment for Graves’ disease. People with TED need to be looked after by an eye specialist (ophthalmologist) and a thyroid specialist (endocrinologist). If you have never had issues with your thyroid, a simple blood test will be ordered to check your thIf you have never had issues with your thyroid, a simple blood test will be ordered to check your thyroid levels.
The pathogenesis of ophthalmopathy is that the immune response to a TSH receptor–like protein in orbital connective tissue initiates cytokine formation, promoting production by orbital fibroblasts of hydrophilic glycosaminoglycans, resulting in increased osmotic pressure, extraocular muscle volume, fluid accumulation and clinical ophthalmopathy.
The pathogenesis of Graves' disease is illustrated. The hyperthyroidism and goitre of Graves' disease are caused by stimulation of the thyroid by TSH receptor antibodies. Production of these antibodies is primarily within the thyroid gland itself, and the immunology underlying this process has been ably described in detail elsewhere. It has been suggested that a genetic clonal lack of suppressor T cells may be responsible for the unregulated production of TSH receptor antibody (TSH = thyroid-stimulating hormone, T3 = triiodothyronine, T4 = thyroxine)
Geometric and Volumetric Measurements of Orbital Structures in CT Scans in Thyroid Eye Disease Classification
Classification of Thyroid Eye Disease (TED) Patients
patients were first divided into two groups of patients with impaired motility (TED-IM) and normal motility (TED-NM).
The diagnostic criteria for TED-IM were as follows:
(1) diplopia;
(2) ocular motility disturbance in physical examination;
(3) restrictive strabismus in synoptophore examination.
Then, to evaluate the effect of enlargement of the extraocular muscle on the optic nerve, all cases in the TED-IM group were categorized into dysthyroid optic neuropathy DON and non-DON groups.
The diagnostic criteria for DON were as follows:
(1) delayed visual evoked potential;
(2) decreased best-corrected visual acuity not associated with other underlying diseases; and
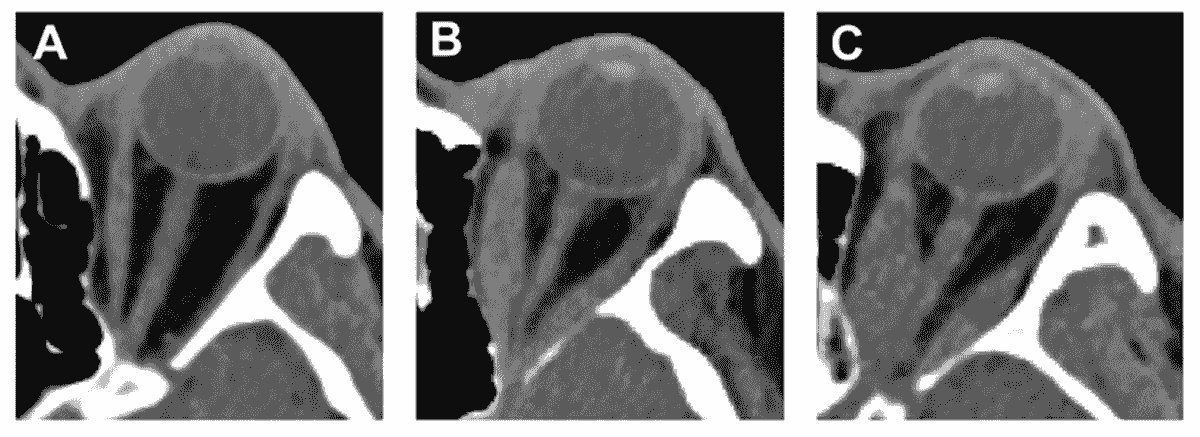
(3) the presence of a visual field defect lower than 5.0 decibels. The representative CT images of TED-NM, TED-IM-Non-DON, and TED-IM-DON are shown in the following figures.
The computed tomography (CT) images of patients with thyroid eye disease (TED) with normal motility (TED-NM) (A), non-dysthyroid optic neuropathy (DON) in impaired motility (IM) group (TED-IM-Non-DON) (B), and TED-IM-DON (C).
Orbital Computed Tomography (CT) Scan
All TED patients, without injecting sedatives or contrast media, were scanned using a high-resolution CT scanner (Somatom Force, Siemens Healthineers, Forchheim, Germany). The CT scans were obtained with contiguous axial slices. Patients were in the supine position and asked to look at a fixed point.
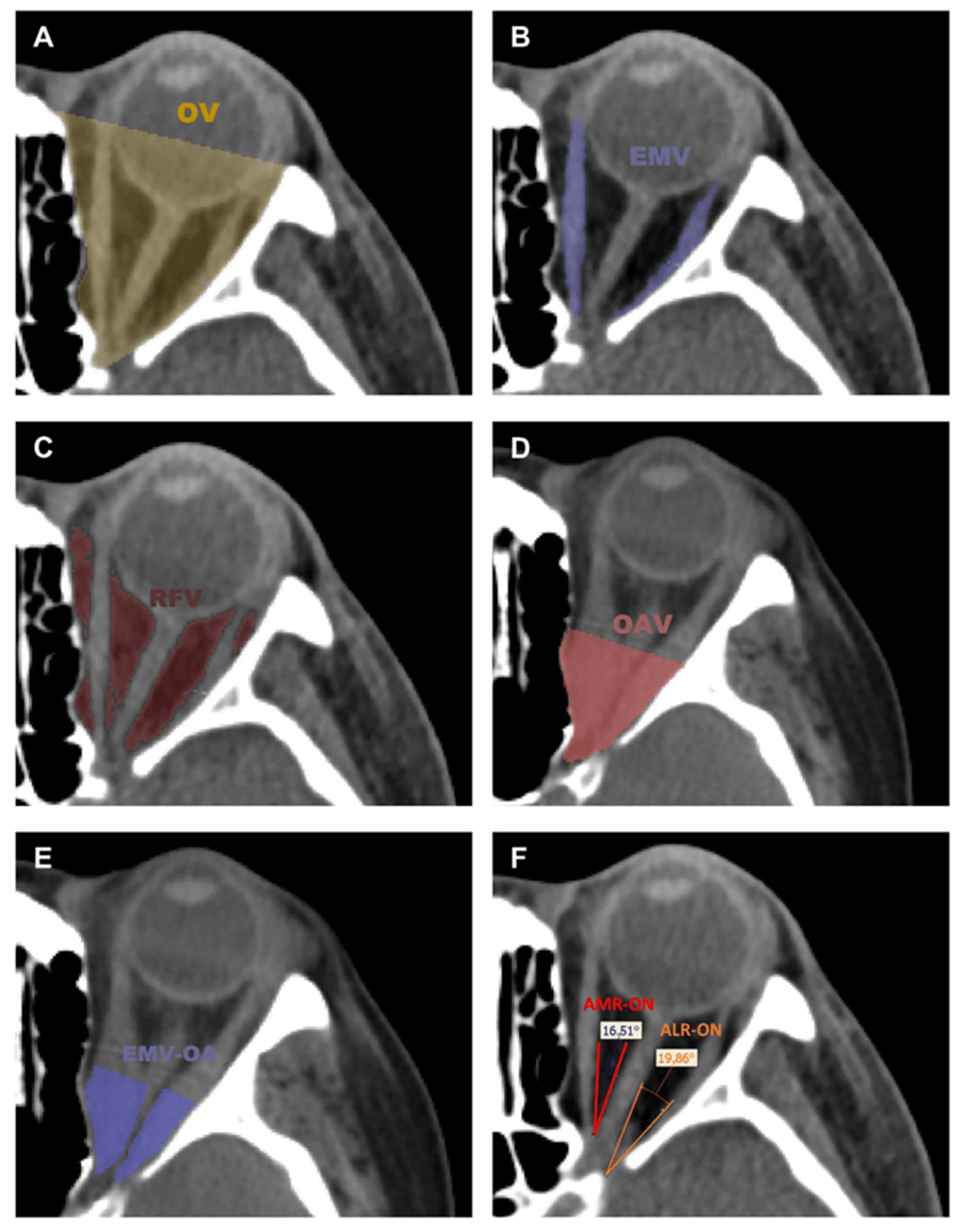
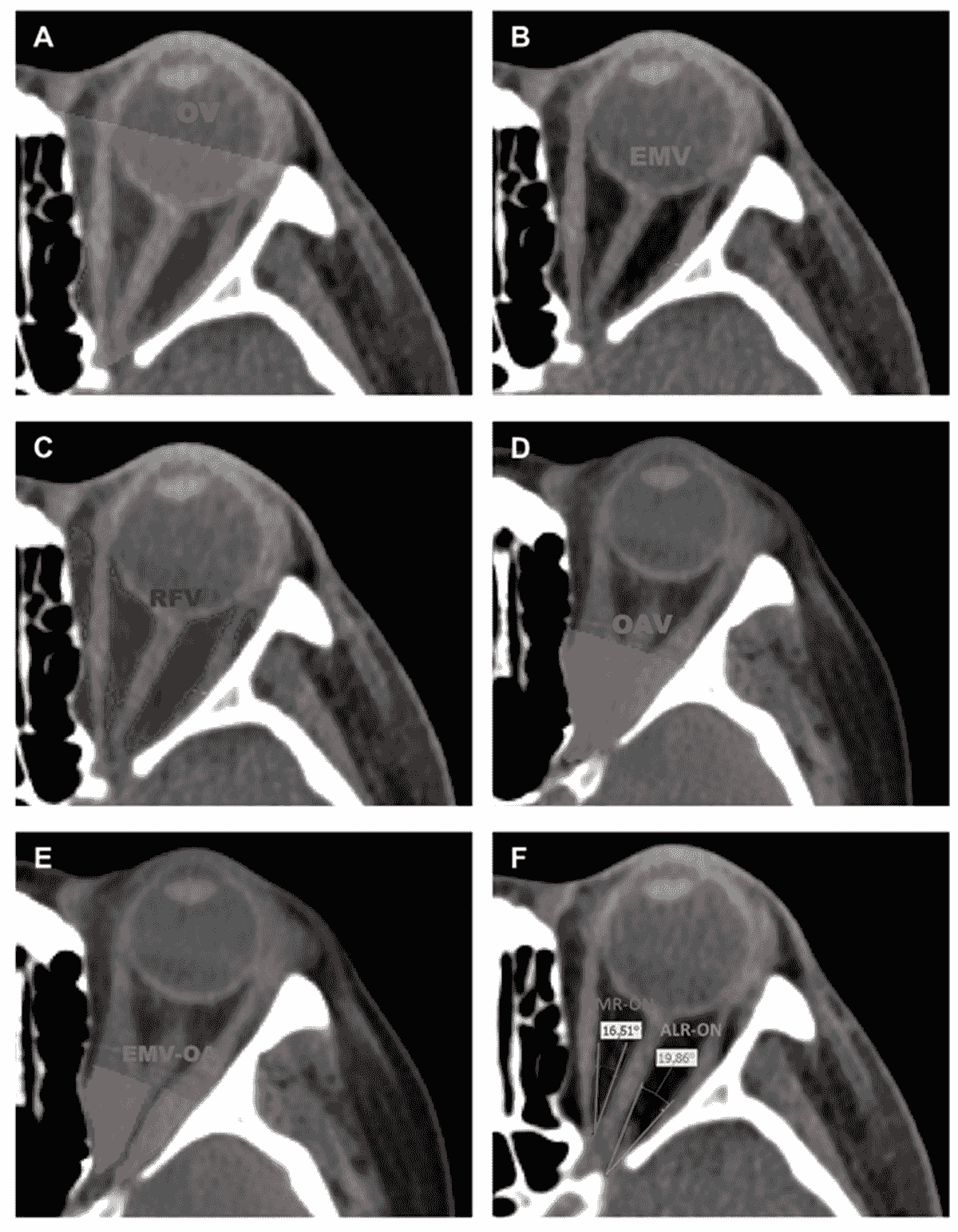
Volume and Angle Measurements of Orbital Tissue
Parameter measurements include orbital volume (OV), extraocular muscle volume (EMV), retroorbital fat volume (RFV), orbital apex volume (OAV), extraocular muscle volume in orbital apex (EMV-OA), the angles between medial rectus and optic nerve (AMR-ON), and the angle between the lateral rectus and optic nerve (ALR-ON) . The extraocular muscles include four muscles as follows: medial rectus, lateral rectus, superior rectus, and inferior rectus.
Axial CT slices with the highlighted segmented tissues. (A) orbital volume (OV), (B) extraocular muscle volume (EMV), (C) retroorbital fat volume (RFV), (D) orbital apex volume (OAV), (E) extraocular muscle volume in orbital apex (EMV-OA), (F) the angle between the medial rectus and optic nerve (AMR-ON), and the angle between the lateral rectus and optic nerve (ALR-ON).
© 2025