Less is more for health and happiness
- …


Less is more for health and happiness
- …


Science helps us to understand and brings hope
Read more...1. Eyes "bulging out" – The eyeball protrudes from its socket, causing the thyroid gland to...Read more...I. First, a review: What are autoantibodies against TSH receptors? Remember in Graves'...Read more...I. First, let's understand: What is Graves' disease? Our bodies have an "immune system...Read more...Let's use the analogy of the thyroid hormone factory again, explaining the relationship between...Read more...1. Thyroid-stimulatinghormone (TSH): The "messenger" of the thyroid gland. It resides in a small...Read more...Thyroid eye disease is an autoimmune disorderclosely related to Graves' disease. It causes...Read more...Background 1.1 Thyroid Eye Disease (TED) Thyroid eye disease (TED) is a disabling condition...Three Musketeers in immune system
APC, MHC, CD4 T cell
How your immune systeme recognize antigen?

APC (Antigen-Presenting Cell): These are immune cells like dendritic cells, macrophages, and B cells that act as "messengers." They detect harmful invaders, process parts of them (called antigens), and present these pieces on their surface to T cells, effectively showing them what to target.
MHC (Major Histocompatibility Complex): MHC molecules are like display stands on the surface of APCs. They hold and present the antigen fragments to T cells. There are different classes of MHC; for CD4 T cells, it's usually MHC class II molecules that present the antigen.
CD4 T Cell: These are a type of immune cell known as helper T cells. They have a special protein called CD4 on their surface, which helps them recognize signals from other immune cells. Their main role is to assist and coordinate the immune response, making sure the body effectively fights off infections.
Cytokine, co-stimulator, CD4 T cell
How your immune systeme recognize antigen?

Proinflammatory cytokine: Proinflammatory cytokine release and bacterial antigen presence trigger the elevated synthesis of MHC-II molecules to maximize the presentation of foreign antigens for an efficient CD4+ T cell response. High IFN-γ levels increase the number of MHC-II molecules on professional and nonprofessional APCs, thereby altering the composition of the MHC peptidome in the inflammatory area
Costimulatory molecules: Co-stimulation is a secondary signal which immune cells rely on to activate an immune response in the presence of an antigen-presenting cell. During the activation of lymphocytes, co-stimulation is often crucial to the development of an effective immune response. Co-stimulation is required in addition to the antigen-specific signal from their antigen receptors. APCs, activated in pathogenic conditions, express an increased number of costimulatory molecules
CD4 T Cell: The development of autoreactive CD4+ T cells in a proinflammatory environment. The proinflammatory environment caused by viral or bacterial infection entails IFN-γ production, which results in increased MHC-II and costimulatory molecule expression compared to normal conditions. Therefore, rare self-antigens are present in a greater number, which can lead to the potential activation of autoreactive T cells.
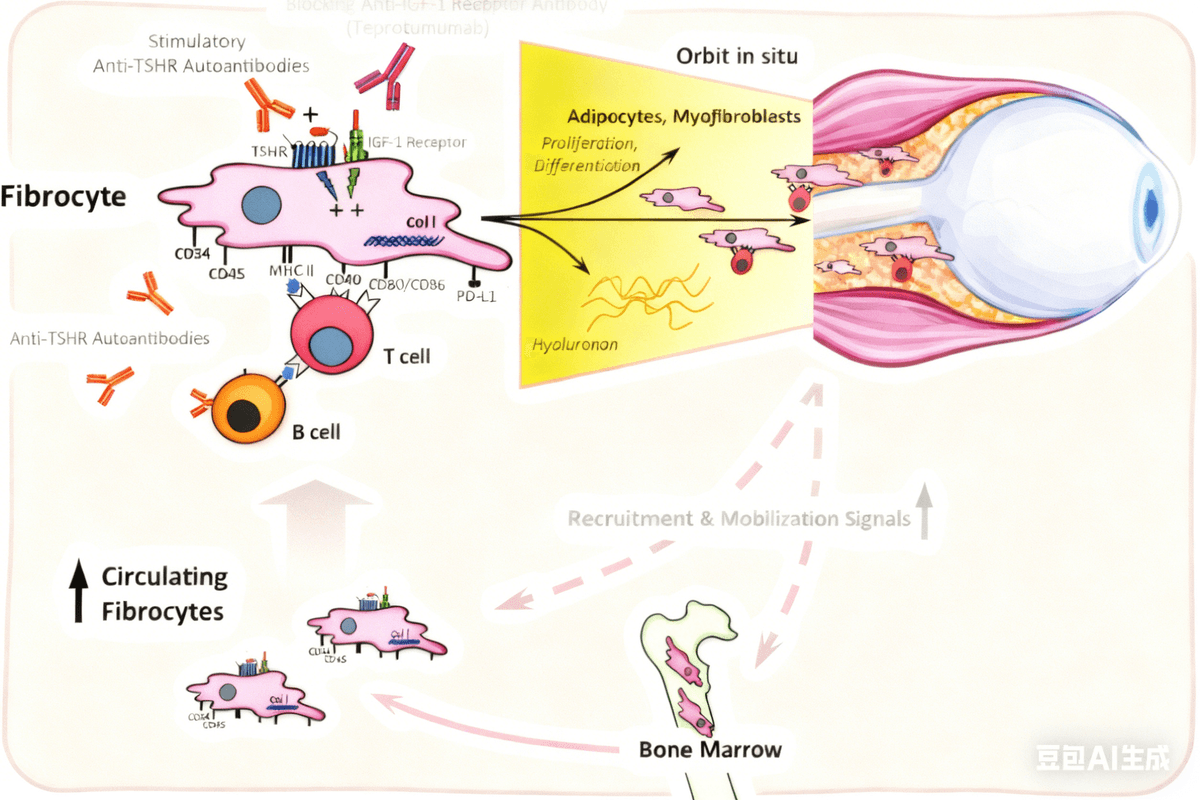
TSHR, IGF1R, Fibroblast
What does TSHR do in my eyes?
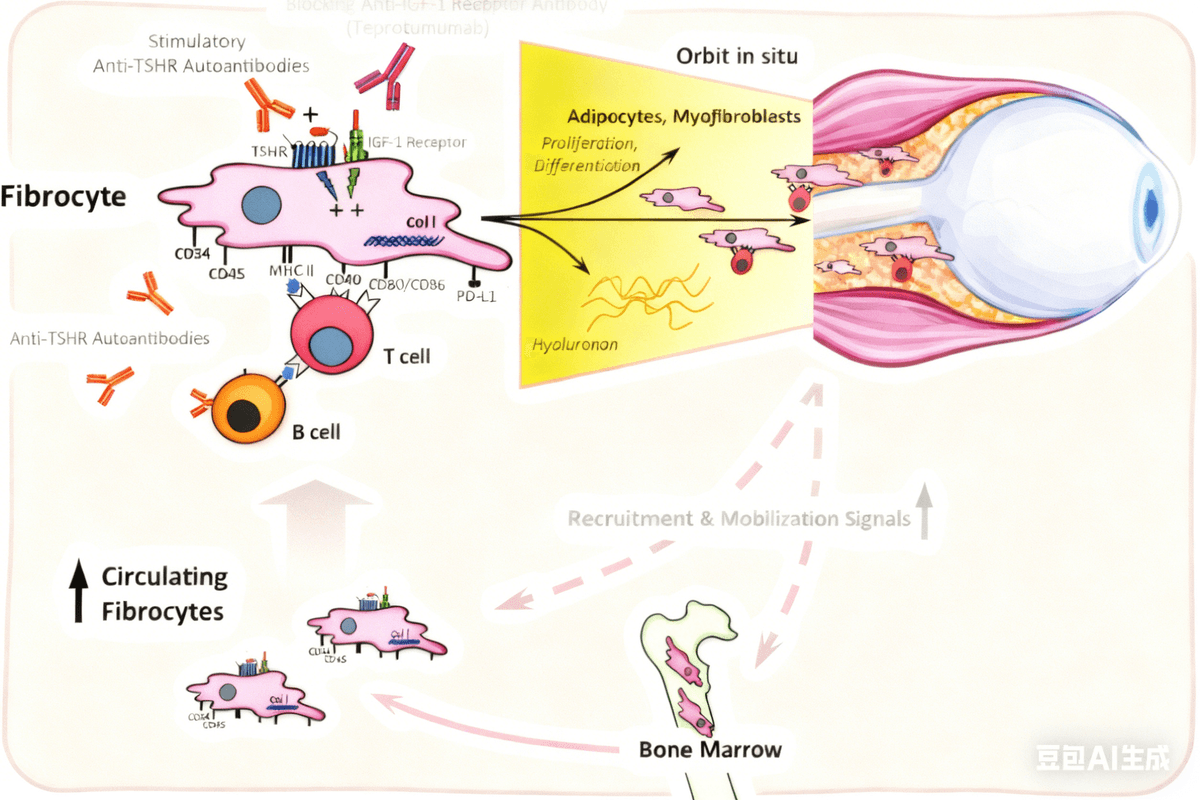
TSHR (Thyroid Stimulating Hormone Receptor)
- Normally, TSHR is found mainly on thyroid cells, where it helps regulate thyroid hormone production.
- In TED, TSHR is also found on orbital fibroblasts (cells around the eyes).
- Autoantibodies from the immune system can mistakenly target TSHR on these orbital fibroblasts.
- This abnormal activation leads to fibroblast proliferation (growth) and production of substances that cause tissue swelling and inflammation behind the eyes.
IGF1R (Insulin-like Growth Factor 1 Receptor)
- IGF1R is present on orbital fibroblasts as well.
- Research shows that in TED, IGF1R forms a complex with TSHR, and both receptors can be activated by autoantibodies.
- Activation of IGF1R contributes to signaling that promotes fibroblast activation, inflammation, and tissue remodeling.
- IGF1R plays a significant role in the abnormal immune response and tissue changes seen in TED.
Fibroblasts
- Fibroblasts in the orbit (eye socket) are the main target cells affected in TED.
- When TSHR and IGF1R on fibroblasts are activated abnormally by autoantibodies, fibroblasts multiply and produce excess glycosaminoglycans (GAGs), molecules that attract water.
- This leads to tissue swelling, increased volume of muscles and fat behind the eyes, causing the characteristic bulging eyes (proptosis).
- Fibroblasts also contribute to inflammation by releasing cytokines, which further exacerbate the immune response.
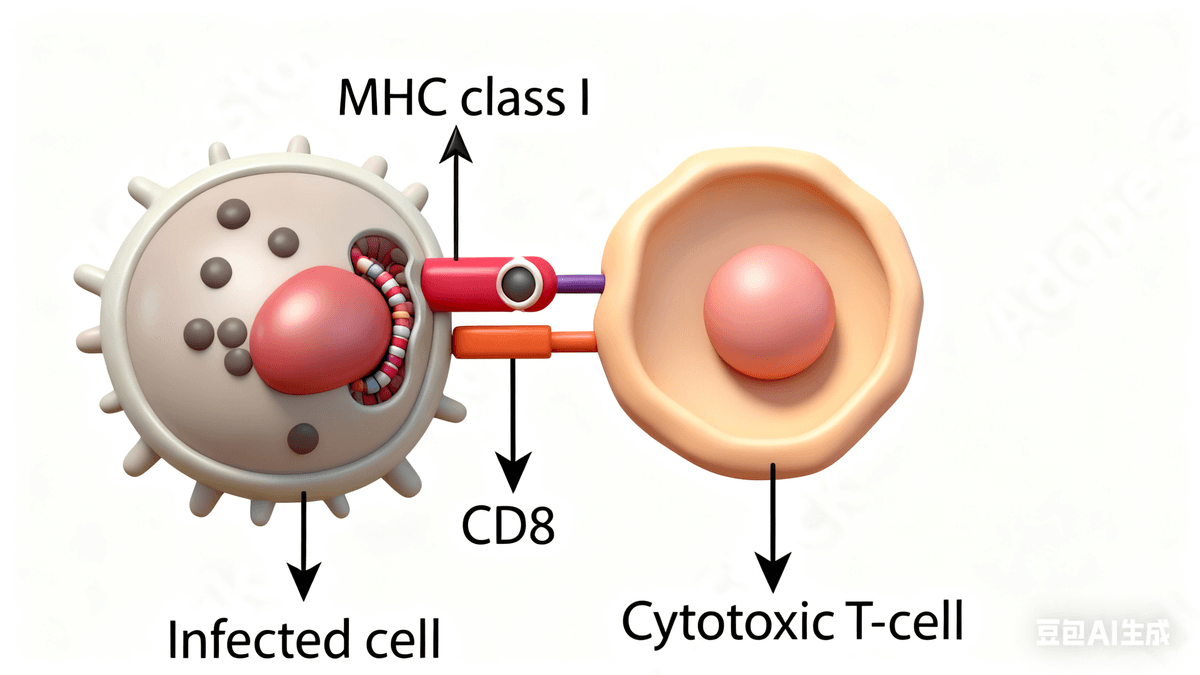
Target cell, MHC, CD8 T cell
How your immune cells recognize foreginers?
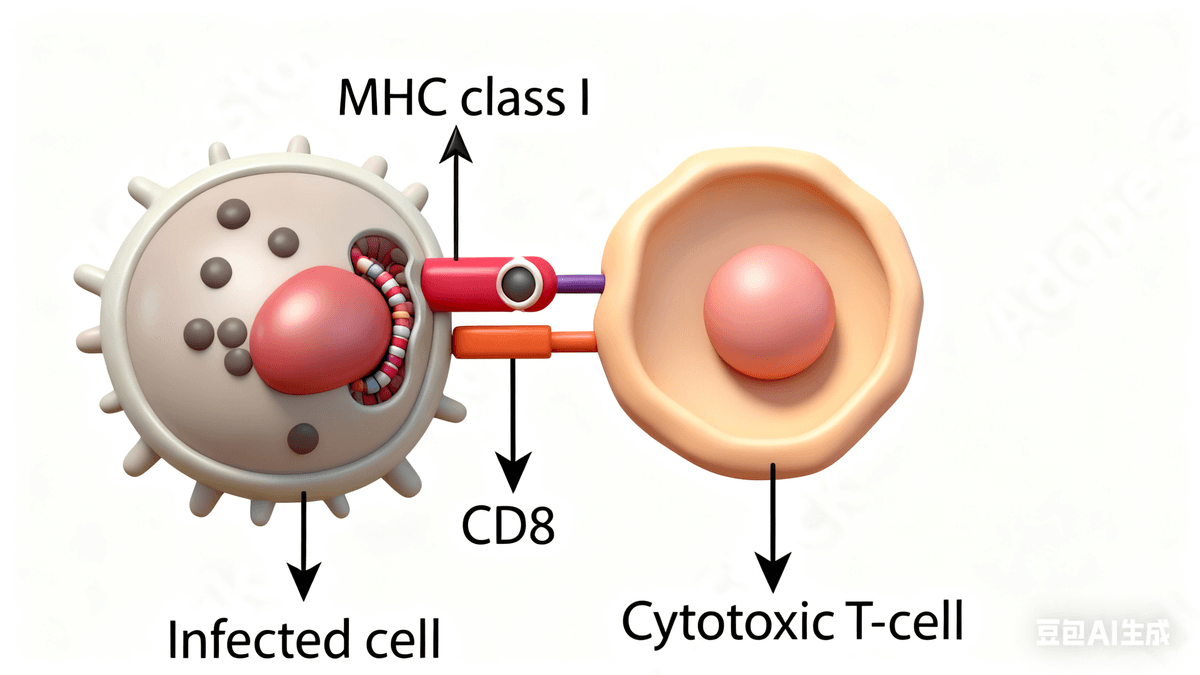
Target Cell: This is a cell in your body that is infected by a virus or has become abnormal (like a cancer cell). The immune system aims to identify and eliminate these target cells to keep you healthy.
MHC (Major Histocompatibility Complex): These are special molecules found on the surface of almost all your cells. They display small pieces of proteins from inside the cell. If a cell is infected or abnormal, MHC molecules show pieces of these problematic proteins to immune cells, acting like a “red flag” to alert the immune system.
CD8 T Cell: Also called cytotoxic T cells, these immune cells have a protein called CD8 on their surface. They “read” the signals presented by MHC class I molecules on target cells. When they recognize something harmful, they can kill the infected or abnormal target cells, helping to protect your body.
Antigen, Plasma cell, Antibody
How your immune systeme know what kind of antibody to produce?
B Cell: B cells are a type of white blood cell that helps protect your body from infections. Their special job is to recognize harmful invaders like bacteria and viruses and help your body fight them.
BCR (B Cell Receptor): This is a protein found on the surface of each B cell. It acts like a unique "antenna" that can recognize and bind to specific parts of a pathogen (called antigens). This helps the B cell know exactly what to target.
Antibody: When a B cell is activated, it can turn into a plasma cell that produces antibodies. Antibodies are Y-shaped proteins that circulate in your blood and other fluids. They can stick to pathogens, marking them for destruction or neutralizing them directly.
Antibody, Antigen, Fc
How does antibody look like?
Antibody: Antibodies are special Y-shaped proteins made by B cells. They recognize and bind to specific harmful substances, called antigens, like bacteria or viruses. By sticking to these invaders, antibodies help neutralize them or mark them for destruction.
Antigen: An antigen is any substance that the immune system recognizes as foreign or dangerous. This can be parts of bacteria, viruses, or other pathogens. Antigens are what antibodies and immune cells "look out for" to protect your body.
Fc: The Fc region is the tail part of an antibody. While the top part (Fab region) binds to the antigen, the Fc region interacts with other immune cells. It acts like a "handle," allowing immune cells to grab onto the antibody and help destroy the marked invader.
CD8, Granzyme, Perforin
How your immune cells attack "bad" guys?
CD8: CD8 is a protein found on the surface of a special group of immune cells called cytotoxic T cells. These cells help protect your body by finding and killing infected or abnormal cells, like those infected by viruses or cancer cells.
Granzyme: Granzymes are powerful enzymes released by cytotoxic T cells. Once these enzymes enter a target cell, they trigger processes that lead to the cell's self-destruction, helping to eliminate infected or harmful cells safely.
Perforin: Perforin is another protein released by cytotoxic T cells. It creates tiny pores or holes in the membrane of the target cell, allowing granzymes to enter the cell and do their job.
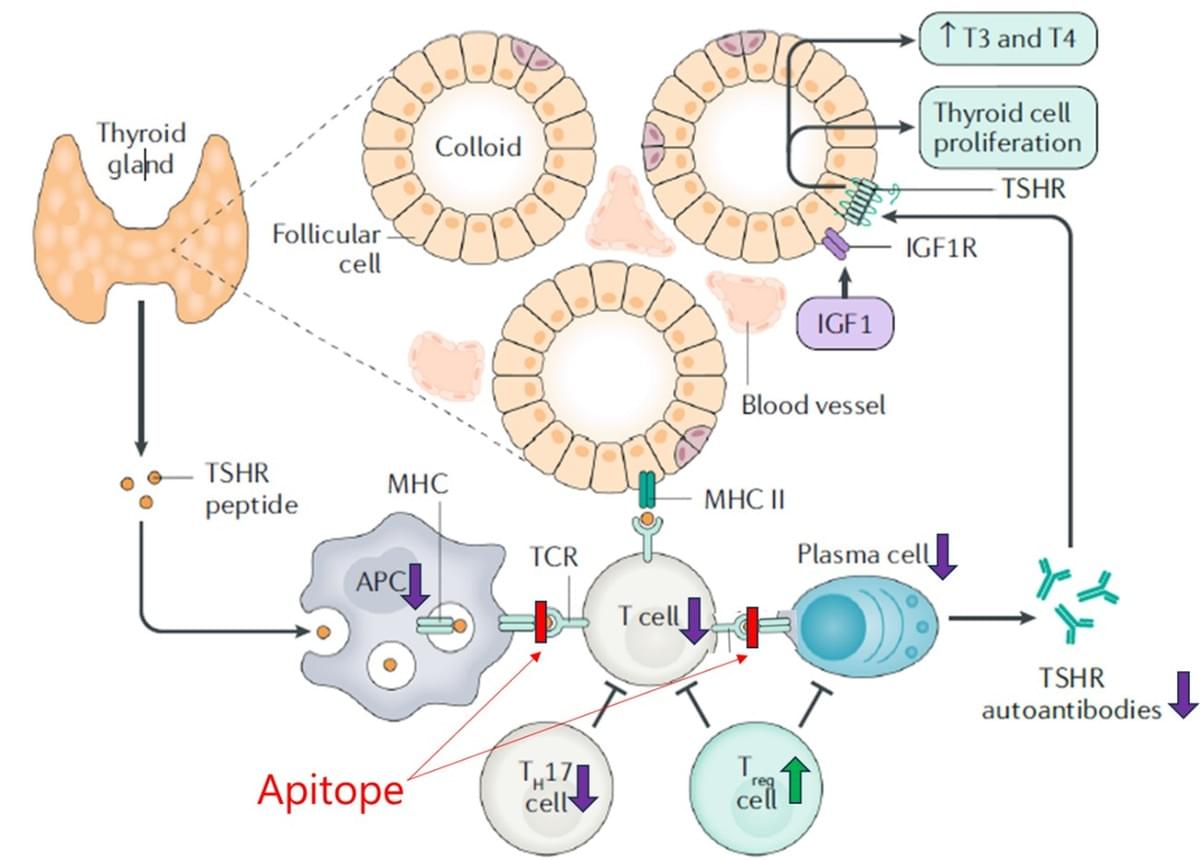
TSH, TSHR, Thyroid hormones
What are thyroid homrones? How they are regulated?
TSH (Thyroid Stimulating Hormone) is a hormone produced by the pituitary gland in your brain. Its main job is to tell your thyroid gland to make thyroid hormones. Think of TSH as a friendly messenger encouraging your thyroid to work properly.
TSHR (Thyroid Stimulating Hormone Receptor) is like a special "lock" on the thyroid gland that fits the TSH "key." When TSH binds to TSHR, it signals the thyroid gland to produce and release thyroid hormones. This interaction helps keep your body's metabolism running smoothly.
Thyroid hormones mainly refer to two hormones: T3 (triiodothyronine) and T4 (thyroxine). These hormones are produced by the thyroid gland and play a wonderful role in regulating your metabolism, energy levels, growth, and development. They influence how your body uses energy, helping you feel active and healthy.
TSHR, TSAb, TBAb
Do I have antibodies against TSHR?
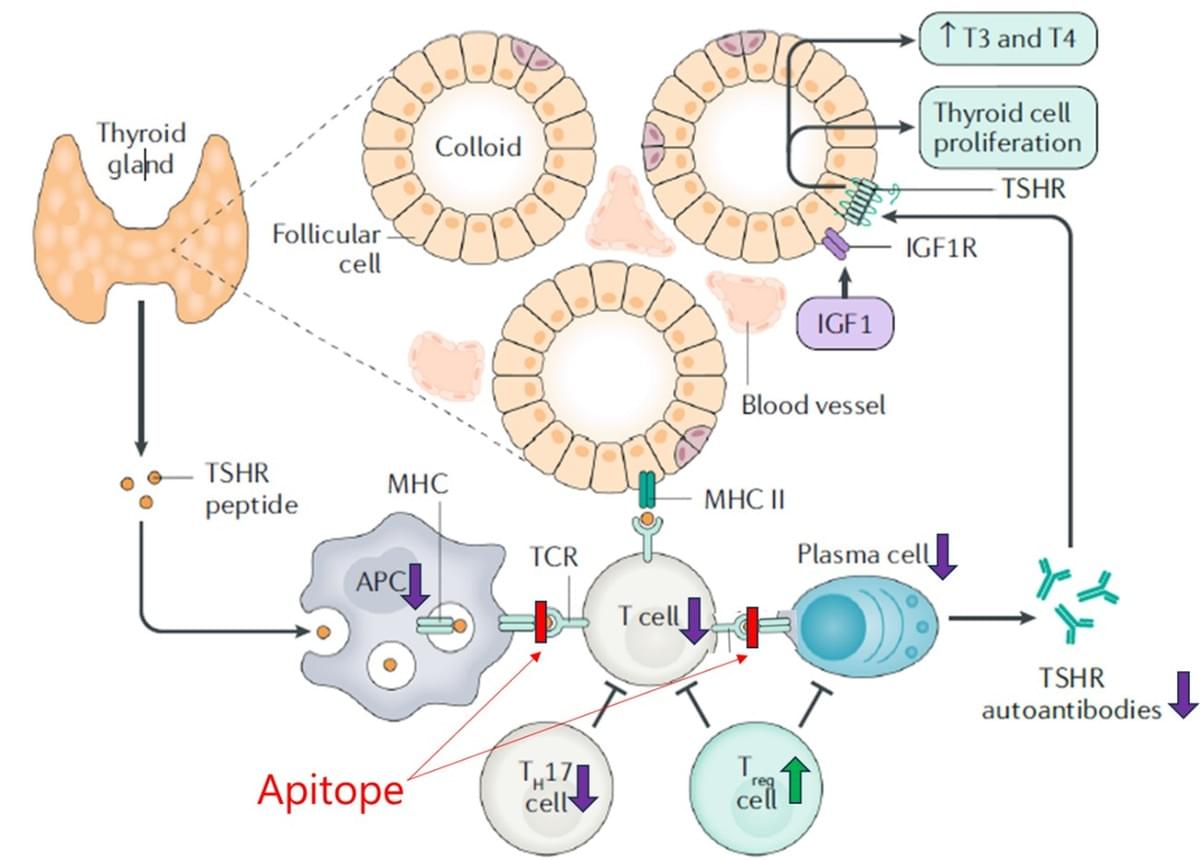
TSHR (Thyroid Stimulating Hormone Receptor):
- TSHR is a receptor normally found on thyroid cells, where it regulates thyroid hormone production.
- In TED, TSHR is also found on orbital fibroblasts (cells around the eyes).
- This receptor becomes a key target in the disease process because the immune system mistakenly attacks it, leading to inflammation and tissue changes around the eyes.
TSAb (Thyroid Stimulating Antibodies):
- TSAb are autoantibodies produced by the immune system that stimulate the TSHR.
- In Graves’ disease and TED, TSAb bind to TSHR on thyroid cells and orbital fibroblasts, activating them.
- This activation causes overproduction of thyroid hormones and stimulates fibroblasts in the orbit to proliferate and produce substances causing inflammation and swelling.
- The action of TSAb is like an overenthusiastic messenger pushing TSHR to work overtime, which contributes to the eye symptoms in TED.
TBAb (Thyroid Blocking Antibodies):
- TBAb are autoantibodies that block TSHR, preventing its activation.
- These antibodies are more commonly associated with hypothyroidism (underactive thyroid) rather than TED.
- In the context of TED, TBAb have a less clear role but generally, they oppose the stimulatory effects of TSAb.
- Understanding the balance between TSAb and TBAb helps doctors grasp the patient's thyroid status and disease activity.
Neuron, MBP, Antibody
How my immunity hurts my nervous system?
Neurons: These are the fundamental nerve cells that transmit electrical signals in your brain and spinal cord. In MS, neurons themselves aren't the primary target, but they can be affected indirectly. The damage to the protective myelin sheath around the neurons slows down or blocks these signals, leading to the various neurological symptoms seen in MS.
Myelin Basic Protein (MBP): MBP is a key protein component of the myelin sheath, which insulates nerve fibers and allows rapid signal transmission. In MS, the immune system mistakenly recognizes MBP as a harmful substance and attacks it. This immune attack leads to degradation of the myelin sheath—a process called demyelination—resulting in impaired nerve function.
Antibodies: These are proteins produced by the immune system that typically help fight infections. However, in MS, certain antibodies are directed against components of the myelin sheath, including MBP. These autoantibodies contribute to the immune-mediated destruction of myelin and may also target other nervous system components, exacerbating the disease process.
Beta cell, MHC I, CD8 T cell
What's particularity about the type 1 diabetes?
Beta Cells: These are specialized cells in the pancreas that produce insulin, a hormone crucial for regulating blood sugar levels. In type 1 diabetes, the immune system mistakenly targets and destroys these beta cells, leading to insufficient insulin production.
MHC Class I (MHC I): These molecules are found on the surface of almost all nucleated cells, including beta cells. They present protein fragments (peptides) from inside the cell to the immune system. In type 1 diabetes, beta cells present abnormal or self-peptides via MHC I, which can trigger immune recognition.
CD8 T Cells: These are cytotoxic T lymphocytes that recognize antigens presented by MHC I molecules. In type 1 diabetes, CD8 T cells recognize peptides presented by MHC I on beta cells as foreign or dangerous, leading them to attack and kill the beta cells.
APC, Peptide, Antibody
Why antibodies are so specific?
APC (Antigen-Presenting Cell): These are special immune cells, like dendritic cells, macrophages, and B cells. Their job is to find harmful invaders (like viruses or bacteria), break them down, and then present small pieces of these invaders, called peptides, on their surface. This process helps alert other immune cells to the threat.
Peptide: A peptide is a small fragment of a protein, often from a pathogen or infected cell. APCs display these peptides on their surface using molecules called MHC, which helps T cells recognize and respond to the invaders.
Antibody: Antibodies are Y-shaped proteins produced by B cells once they've been activated. They specifically bind to pathogens or their toxins, neutralizing them or marking them for destruction by other immune cells.
© 2025